November 2020 | Volume 22 No. 1
COVID-19: Tracking the Pandemic
POOR VENTILATION HELPS THE VIRUS SPREAD
HKU’s Department of Mechanical Engineering has shown that COVID-19 can be transmitted several metres by air when there is poor ventilation – a timely warning as winter approaches and people spend more time indoors.
The finding came out of a detailed study of three COVID-19 outbreaks in crowded situations that looked at where infected individuals were located, who they infected and the rate of ventilation. The outbreaks were at a Guangzhou restaurant, two Hunan buses, and the Diamond Princess cruise ship from January to March, and the study was led by Professor Yuguo Li, Chair Professor of Building Environment, who previously played a key part in showing the role of ventilation in two clusters of cases during the 2003 SARS outbreak.
At the Guangzhou restaurant, three families who did not know each other were sitting at adjacent tables. An index patient sat at one table and subsequently infected nine people at all three tables, including one person who sat 4.6 metres away. Subsequent measurements by Professor Li and his team showed the ventilation rate was only 1 L/s (one litre per second) per person, against the international standard of 5 L/s.
Similarly, the Hunan buses were poorly ventilated. One index patient took a bus ride of three hours and 20 minutes that resulted in seven patients being infected, then took a second one-hour journey on a minibus in which two people were infected. The furthest infected person was 9.5 metres away from the index patient. The bus had a time-averaged ventilation rate of 1.7 L/s and the minibus 3.2 L/s
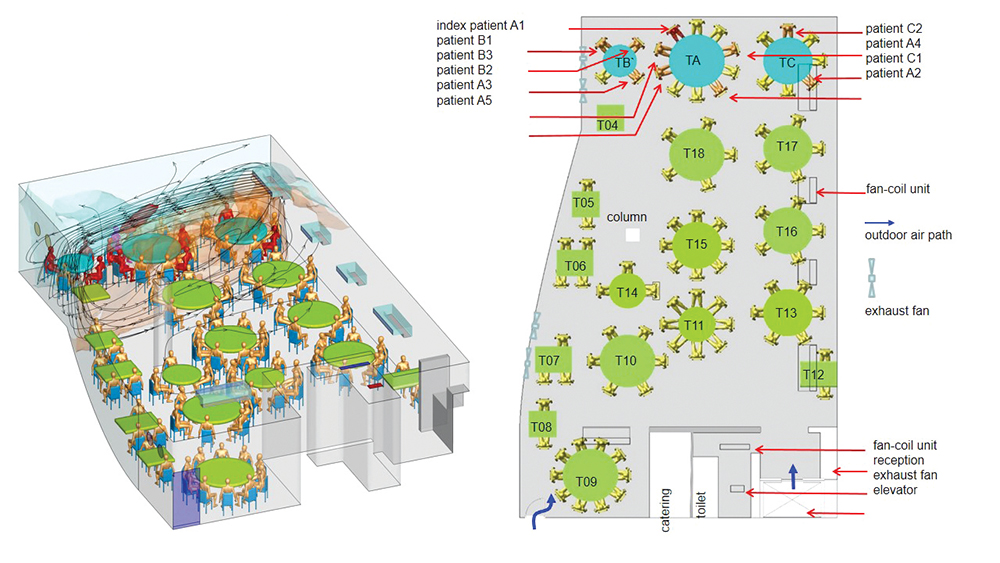
The path of airflow between the tables of the three families involved in the Guangzhou restaurant case.
Keep the air moving
On the Diamond Princess, which had more than 700 confirmed cases, the findings went the other way: the team showed that infection among passengers after the onset of quarantine was limited to those who had stayed in the same stateroom as an infected passenger. This probably meant the central air-conditioning system did not play a role, although the team were unable to get reference measurements.
“In a sufficiently ventilated room, droplet concentrations in the exhaled jet of air from an infected person will continually decrease and become indistinguishable from background room air at a distance of about 1.5 metres. Our findings suggest that airborne transmission of the COVID-19 virus Professor Li is an expert in ventilation of indoor environments with a focus on environmental transmission of diseases. The path of airflow between the tables of the three families involved in the Guangzhou restaurant case. indoors is likely when the ventilation rate is less than 3 L/s per person,” Professor Li said.
Public places should enhance indoor air ventilation and social gatherings indoors should be avoided if there is not sufficient ventilation, he said. A carbon dioxide sensor could help indicate poor ventilation if the reading is more than 1,000 parts per million. Otherwise, “a simple criterion for insufficient ventilation is if you can smell other people’s breath from a distance,” he added.
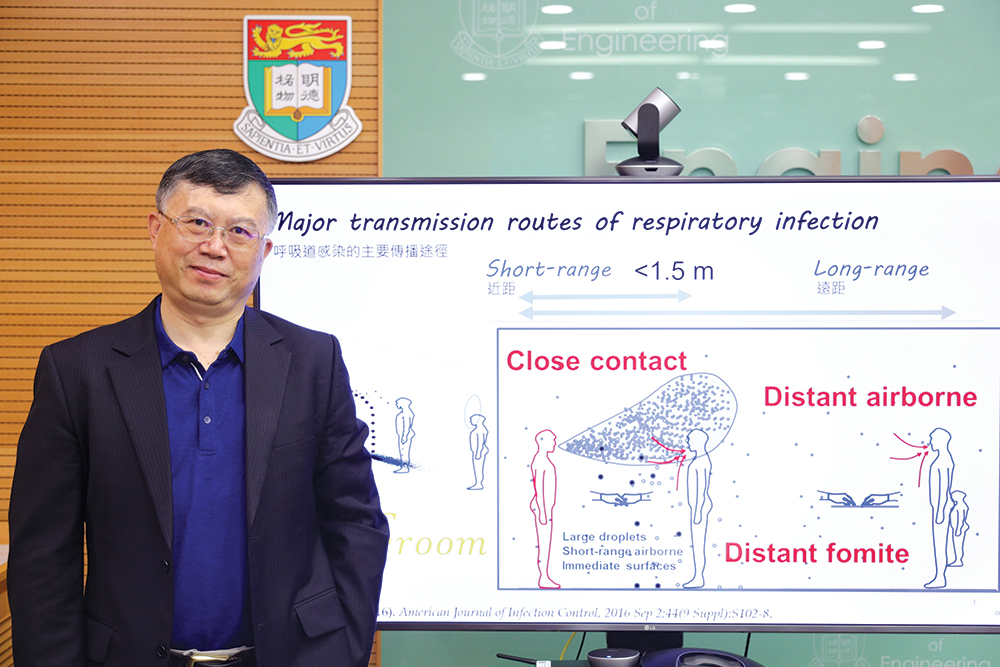
Professor Li is an expert in ventilation of indoor environments with a focus on environmental transmission of diseases.
A simple criterion for insufficient ventilation is if you can smell other people’s breath from a distance.

PROFESSOR YUGUO LI
USING PHONE DATA TO TRACK A PANDEMIC
A team of business and statistics researchers, with little background in medicine, have developed a model to accurately predict COVID-19’s spread and assess risk using only mobile phone data, and to explore people’s response to the pandemic.
The team, led by Dr Jayson Jia Shi of the Faculty of Business and Economics, focussed on Wuhan, the epicentre of the COVID-19. Complex mathematical models had shown, in retrospect, how the virus spread to the rest of the country and the world. But Dr Jia and his colleagues found a simpler, real-time path to the same conclusion with mobile phone data.
Phones automatically alert cell towers whenever they are in range, making them useful for showing population movement. Dr Jia and his collaborators had access to anonymised mobile phone data from China’s telecom companies and used it to track COVID-19’s spread.
They showed that from January 1 this year to January 24, when Wuhan was quarantined, more than 11 million people travelled through the city on their way to 296 prefectures on the Mainland. This information was fed into a model that also captured the number of COVID-19 cases in each place. The results confirmed what these places experienced: the traffic of people from Wuhan predicted how fast their case load grew. The findings were published in Nature at the end of April.
“Our model captured 96 per cent of the statistical variance in the growth of COVID-19,” he said. “By establishing this relationship, we could also predict about two weeks into the future with good accuracy.”
They received proof of this while still in the midst of the study, when they noticed that Wenzhou in Zhejiang province was reporting far fewer cases than predicted by the number of arrivals from Wuhan. A short time later, the reported cases started rising and Wenzhou imposed quarantine conditions.
“Our paper established the basic assumption that you can use movement data to infer that there are going to be more imported cases,” he said. Their efforts resulted in a COVID-19 risk modelling toolkit and other scholars have picked up on the findings to explore the relationship further.
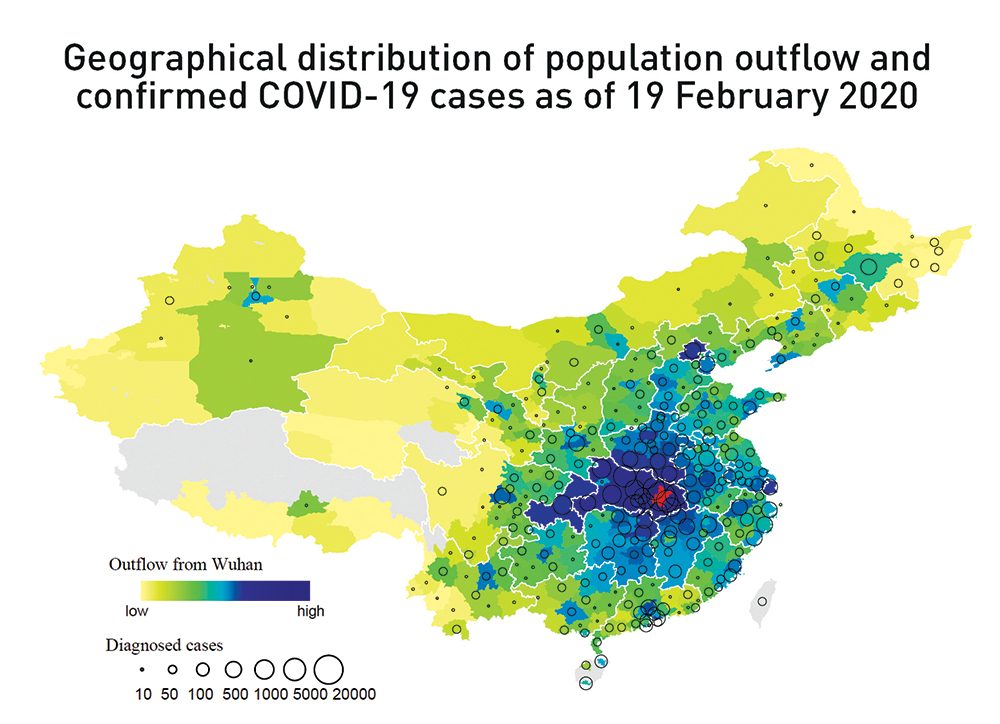
There is a high overlap between the geographical distribution of aggregate population outflow from Wuhan until January 24, 2020 (in red) and the number of confirmed cases of COVID-19 in other Chinese prefectures (n = 296 prefectures). (Map source: National Catalogue Service for Geographic Information. Grey areas lack population outflow data.)
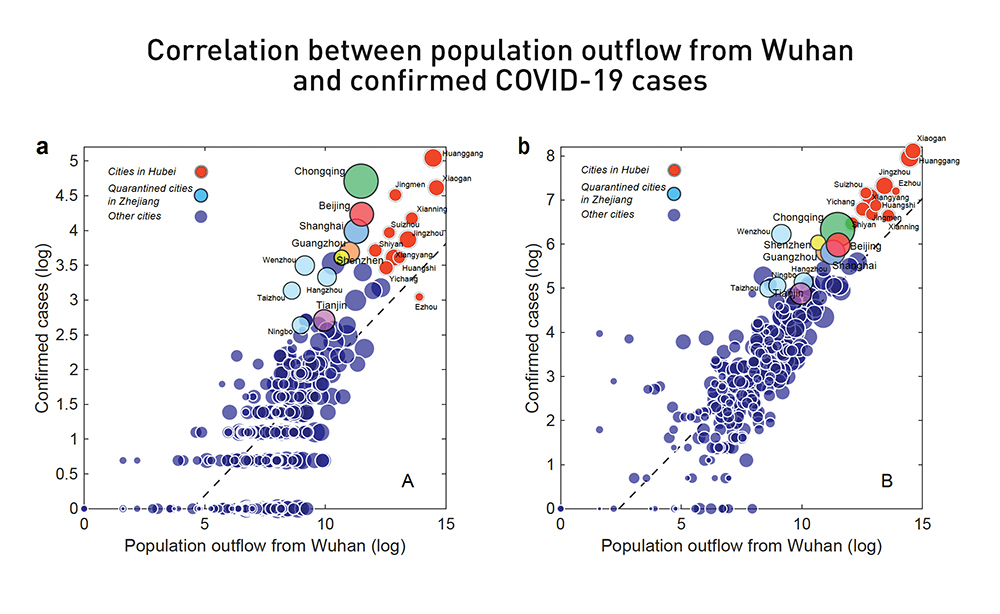
The relationship between the log-transformed aggregate population outflow from Wuhan (up to January 24, 2020) and the log-transformed number of confirmed cases by prefecture on January 26, 2020 (a) and February 19, 2020 (b). Red circles are prefectures in Hubei; light blue circles are four quarantined prefectures in Zhejiang (including Wenzhou); and the six largest prefectures in China are indicated with unique colours.
Coping behaviour
Dr Jia is now looking at another aspect of mobile phones, the use of apps, to explore COVID-19’s impact on people’s behaviour. This follows on from earlier research he did on the 2013 Ya’an earthquake in Sichuan.
That study focussed on social networks and used data from family phone plans to see who people called right after the earthquake hit (mainly family members, rather than the people they called most frequently prior to the tremor, who are presumably work colleagues and friends). It then went a step further to look at which apps people used in the wake of the quake.
Apps were divided into three categories – information related (such as news and banking apps), communications (such as WeChat) and hedonic (such as games, video and music). The data showed that people who lived closest to where the tremor was strongest increased their use of hedonic apps in the following week. Moreover, the use of hedonic apps was associated with less fear about future earthquakes, as revealed in a survey carried out around the same time.
“That was really the surprising finding – the more they engaged in hedonic behaviours, the lower their perceived risk was. The use of these apps was an effective coping behaviour,” Dr Jia said.
“Mobile apps are a way of using digital behaviour to infer what’s on people’s minds, so now we’re using the shock of the pandemic to study lifestyle changes.”
Applying that approach to COVID-19, Dr Jia and his team have been analysing data from Chinese users and the longer-term consequences of less physical mobility and social mixing. Compared to before the pandemic, people have become more reliant on some apps, for example short form video and food delivery apps (no surprise there), and they have changed the way they look at other apps, for example dating apps which previously were correlated with information apps but are now more associated with entertainment apps.
There have also been some positive changes as people make greater use of learning and studying apps, job search apps, and exercise apps (and presumably exercise more). These findings are still in raw form and the implications will need further analysis.
Dr Jia is also trying to promote the idea of social networks when considering the risk factors of COVID-19. “Researchers used to study risk from an atomistic perspective, such as focussing on an individual’s fears or what they thought they could do about a situation. But little thought has been given to social networks and how risk is sometimes beyond our personal control. Let’s say you are really careful about going out, but a family member isn’t. That person is exposing you to risk. So conceptually, we are trying to introduce the idea of networks to risk perception,” he said.
Mobile apps are a way of using digital behaviour to infer what’s on people’s minds, so now we’re using the shock of the pandemic to study lifestyle changes.

DR JAYSON JIA SHI
RECENT COVID-19 RESEARCH ADVANCES
HKUMed scholars have made world’s-first discoveries on COVID-19 and are forging a path towards deeper understanding and control of the disease. Selected highlights in recent months* include:
• Vaccine candidate approved for clinical trial: A flu-based vaccine developed by the State Key Laboratory of Emerging Infectious Diseases in partnership with Xiamen University and Wantai Biopharmaceutical company, was approved for clinical trial in humans in September by China’s National Medical Products Administration. This is the world’s first nasal spray COVID-19 vaccine to be tested in humans.
• First proof of reinfection of COVID-19 virus: Scientists in the Department of Microbiology documented the first case in which a recovered patient was re-infected with SARS-CoV-2, the virus that causes COVID-19, a finding that has important implications for understanding immunity and vaccination prospects for the disease. The case involved a young and apparently healthy patient who was diagnosed with the disease for a second time, four and a half months after the first episode. Samples taken from the patient showed the viral genomes in each case belonged to different lineages.
• New knowledge about transmission dynamics: HKUMed scholars were involved in studies confirmed that virus shedding could begin several days before the first symptoms appeared. They also showed non-pharmaceutical interventions against COVID-19 and influenza, such as testing, contact tracing and population behavioural changes, could be effective controls with less disruption than a total lockdown. Another study found such interventions could shorten the serial interval of the virus over time, which can reduce the chance of transmission. An international study with HKUMed scholars showed containment measures were nonetheless effective, too, lowering the daily increase of new cases to less than five per cent within one month.
• Potential drug targets and candidates identified: An international team identified neutralising monoclonal antibodies as potential therapeutic and prophylactic options against COVID-19. A separate study showed the disease impairs dendritic cell and T cell function, which are involved in human immune defences and could be targets for treatment and vaccine development. An international study of 12,000 known drugs found 13 could be potential candidates for treating COVID-19. Another study identified potential targets for broad-spectrum antiviral drugs to treat COVID-19 and other viral infections (namely, the P9R alkaline peptide and YxxØ-motif).
• Symptoms and effects: The SARSCoV-2 virus was shown to infect neural progenitor cells and brain organoids and intestinal cells. Scholars also found that the eyes may be an important route of human infection.
• Animal connections: Research shows SARS-CoV-2 was probably circulating unnoticed in bats for decades, and that it demonstrably infects bat intestinal cells, as well as those of humans. Tests on two dogs diagnosed with COVID-19 suggested they had been infected via humans.
* From mid-April to mid-September 2020. See here for earlier findings.
For comprehensive and regularly updated reports on our substantial body of COVID-19 research, please visit:

